I was just reading an article about BMI and why it should no longer be used as an accurate measure of obesity. This article reminded me of one of my friends who was upset a few months ago when her doctor said she was classified as “Obese.” I was looking at her and thought – she may be a little overweight but she’s most certainly not obese!
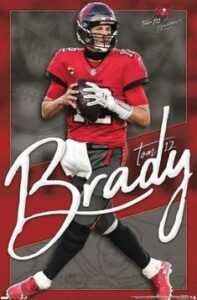 So, being me, I began looking at more research and found that, indeed, BMI alone is not a good indicator for obesity. The BMI measurement tool does not take enough other health factors into consideration; an example of this (that my Patriots fan readers will enjoy) is Tom Brady. According to his BMI – Tom would be classified as overweight – NOT! Here’s a photo of a recent poster that I found of Brady – what do you think?
So, being me, I began looking at more research and found that, indeed, BMI alone is not a good indicator for obesity. The BMI measurement tool does not take enough other health factors into consideration; an example of this (that my Patriots fan readers will enjoy) is Tom Brady. According to his BMI – Tom would be classified as overweight – NOT! Here’s a photo of a recent poster that I found of Brady – what do you think?
BMI is a measurement of your weight to height ratio. The problem is that this measurement does not take into account the amount of lean muscle you have, if you are Tom Brady, nor the weight of your bones, if you are a big boned person like my friend.
Rexford Ahima, MD, PhD, Professor of Medicine and Director of the Obesity Unit at the Institute for Diabetes, Obesity and Metabolism has said:
There is an urgent need for accurate, practical and affordable tools to measure fat and skeletal muscle, and biomarkers that can better predict the risks of diseases and mortality. Advances to improve the measurement of obesity and related factors will help determine the optimal weight for an individual, taking into account factors such as age, sex, genetics, fitness, pre-existing diseases, as well novel blood markers and metabolic parameters altered by obesity.
Research published in 2016 suggested 54 million Americans had been categorized as overweight or obese, but cardiometabolic measures showed they were healthy. Another 21 million had been categorized as “normal” in terms of BMI but were unhealthy.
When it comes to BMI, all races and ethnicities are lumped together — and that can lead to unclear and confusing results. More and more research shows that genetic differences cause biological differences in the relationship between weight, muscle mass, and disease risk among different groups of people. Again, BMI does not account for that.
Certain genetic factors can affect BMI accuracy because of their effect on weight distribution and muscle mass. For example, a 2011 study showed that Black women had less metabolic risk at higher BMIs than White women. Another showed that Mexican American women tend to have more body fat than White and Black women.
Other research shows that for people of Asian or Middle Eastern descent, even a lower BMI may be misleading. They have a higher risk for metabolic diseases like diabetes at a lower BMI than people of European descent.
With so many flaws using BMI as the only measurement and so many newer, more accurate tests to determine if a person is obese or not, why then, are doctors still telling many patients that they are obese, when, in many cases, they are not?
The bottom line here is that we all need to continue to be “the CEO of your own health.” If your doctor is telling you something that you think may be incorrect, get a second opinion! YOU know your body more than someone who sees you once or twice a year and spends a total of 10-20 minutes annually with you!
As we age, we need to concentrate on building more lean muscle, that’s how we’ll stay more fit into our old age.
Do the exercises that you know help you build muscle, make the contents of your plate as colorful as possible with more veggies than carbs and protein, and get 150 minutes a week of brisk walking or dancing, or your favorite aerobic exercise! Have fun with it!
If you’re looking for somewhere to start, here are two videos of modifications to push-ups that you can try! Push-ups help build upper body strength, which is something that many older women do not have much of, so c’mon, join me!
Best of Health,
Kathi




